Abdominal pain has a wide differential. It is broadly classified into acute and chronic. Although a clear differentiation is not well defined it is generally accepted that >6 weeks is deemed chronic. It is also important to recognize an acute/surgical abdomen in a timely fashion and arrange appropriate speciality involvement. In women with abdominal pain always suspect a gynecologic etiology of the abdominal pain, rule on pregnancy ,and do a pelvic examination if appropriate.
History[]
- ChLORIDE FPP: characteristic, location, onset, radiation, intensity, duration, events preceding, frequency, provoking factors, palliating factors
- Fever, N/V, weight loss, night sweats, rash
- History of trauma
- Bowel movements/flatus/diarrhea/constipation blood in stool/ caliber of stool
- Urinary symptoms: hematuria, urge, frequency, dysuria, discharge
- LMP (female), PV discharge, sexual partners, pregnancy
- PMHx: ischemic risk factors, MI, pancreatitis, nephrolithiasis, IBD, ectopic, PID, AAA, diverticulitis
- Past Surgical Hx: bowel surgeries (gallbladder/appendix, etc)
- Past Obs/Past Gyne History
- Medications: NSAID, steroids, OCP/mirena
- Social history: smoking, ETOH, rec drugs
Physical[]
- ABCs + Vitals
- General: dehydration, discomfort
- Abdominal exam: ausculate for bowel sounds), percuss, palpation (light/deep)- masses, rebound, guarding, peritoneal signs
- +/- Genitals: pelvic, testicles
- +/- DRE: masses, rectal tone, blood
- +/- Extra-stigmata of liver disease
Differential[]
RUQ[]
- Hepatitis, gall bladder disease, right lower lobe pneumonia, intestinal ischemia, appendicitis, liver abscess, liver/pancreatic/biliary cancer, pyelonephritis, urinary calculi, trauma or MSK pain, abdominal abscess, herpes zoster, dyspepsia
Epigastric[]
- Dyspepsia, PUD, GERD, gastritis, myocardial infarction, pneumonia, pancreatitis, pancreatic Ca, gall bladder disease, esophageal rupture, gastric volvulus, aortic dissection
LUQ[]
- Gastritis, pancreatitis, PUD, LLL pneumonia, MI, pyelonephritis, ruptured spleen, splenic infarct, diverticulitis, trauma/MSK
Periumbilical[]
- obstruction, gastroenteritis, pancreatitis, aortic dissection, MI, early appendicitis
RLQ[]
- Appendicitis, IBD, IBS, PID, ovarian torsion, ruptured ovarian cyst, tubo-ovarian abscess, endometriosis, ectopic, mittelschmerz, cystitis, hernia, testicular torsion, epididymitis, prostatisis, diverticulitis, urinary calculi, obstruction, AAA, mesenteric adenitis, trauma/MSK, abdominal abscess
LLQ[]
- Diverticulitis, colitis, constipation, obstruction, IBS, gyne (ovarian torsion/cyst/PID, ectopic, endometriosis, mittelschmerz), intestinal ischemia, cystitis, hernia, testicular (torsion, epididymitis), prostatitis, urinary calculi, trauma/MSK, AAA
GI Tract[]
- Infectious/Inflammatory: IBD, gastroenteritis, gastritis, esophagitis, appendicitis, colitis, diverticulitis
- Obstruction: small bowel obstruction, large bowel obstruction, malignancies, volvulus, hernia, intussusception, constipation, adhesions
- Digestion: peptic ulcer disease, lactose intolerance, celiac disease, food allergies, functional dyspepsia
- Other: hemorrhoids, mesenteric ischemia, IBS
Hepatobiliary[]
- Hepatic: hepatitis, hepatic abscess, malignancy, hepatic vein thrombosis
- Gallbladder: cholelithiasis, cholecystitis, choledocholithiasis, malignancy
- Pancreas: pancreatitis, pseudocyst, malignancy
Renal/Bladder/Urinary System[]
- Pyelonephritis, kidney stones, cystitis, urinary retention, malignancy
- Testicular torsion, epididymitis, prostatitis
Gynecologic[]
- PID, ovarian torsion, tubo-ovarian abscess, ovarian cyst, endometriosis, fibroids, ectopic, spontaneous abortion, menstruation, mittelschmerz, malignancy, uterine rupture
Vascular[]
- AAA, aortic dissection, vasculitis, thrombosis/embolism, mesenteric ischemia
Other[]
- MSK pain/strain/trauma
- Neurogenic pain: zoster, nerve entrapment
- Referred pain: pneumonia, PE, MI, pericarditis, spine, testicles
- Metabolic: DKA, uremia, withdrawal
Investigations[]
- Depend on history and physical
- Can include: CBC, lytes, BUN, Cr, LFTs, bilirubin,lipase, amylase,glucose, lactate, T+S, TTG, anti-IgA, ESR/CRP, urine R+M, urine C+S, urine or serum BhCG, +/- septic w/u
- Plain film (3 views of abdomen): free air, obstruction
- Ultrasound: biliary tree, liver, gynecologic, testicular, AAA, hydronephrosis, appendicitis (young,thin)
- CT adbdomen
- Further investigations: ERCP/MRCP, MRI abdo, colonoscopy, endoscopy
Inflammatory Bowel Disease[]
Crohn's disease[]
- Pathophysiology: transmural inflammation of GI tract
- Clinical: crampy abdominal pain, prolonged diarrhea +/- blood (often occult), fatigue, weight loss, +/- fever
- Can be associated with:
- strictures and SBO
- fistulas (communications often between intestine and bladder/skin/bowel/vagina - enterovesical/enterocutaneous/enteroenteric/enterovaginal)
- abscess
- perianal disease: pain, drainage, anal fissure, perirectal abscesses, anorectal fistulas
- malabsorption (bile acids)
- Other GI involvement: amphthous ulcers, odynophagia, dysphagia
- Extraintestinal manifestions: arthritis (sacroilitis, ankylosing spondylitis), eye (uveitis, iritis, episcleritis), skin (erythema nodosum, pyoderma gangrenosum, primary sclerosing cholangitis, renal stones, osteoporosis, vitamin B12 deficiency, venous/arterial thromboembolism, cholelithiasis, Fat soluble vitamin malabsorption (ADEK), pulmonary (bronchiectasis, ILD)
- Investigations:
- CBC, lytes, Cr, Liver enzymes, blood glucose, ESR, CRP, iron studies, B12, albumin (CRP levels correlate with crohn's activity)
- Consider celiac serology, stool testing for culture, ova and parasites, c.diff (pending history)
- Colonscopy with biopsy
- CT: strictures
- MRI: perianal fistulas
- Small bowel disease: upper GI series with small bowel follow-through (barium study - string sign, cobblestoning), CT, CTE, MRI, MRE, enterocysis
- Prognosis: May have slight increase risk of colorectal cancern, no change in mortality. Typical course: exacerbations and remissions. Not medically or surgically curable
- Treatment:
- Depends on severity
- Adults: Crohn's Disease Activity Index (CDAI) and the Harvey-Bradshaw Index (HBI)
- Pediatrics: Pediatric Ulcerative Colitis Activity Index (PUCAI)
- 5 -ASA (mild-moderate) - although poor evidence (Sulfasalazine, mesalamine). Recommended as maintenance therapy.
- Steroids (flare-up): prednisone/budesonide
- Immunosupressants: azathioprine (imuran), MTX - treat active inflammation, maintain remission
- Antibiotics (Metronidazole) for decrease disease activity, perianal disease, fistula, abscess
- Immunomodulators/biologics: infliximab - remicade, adalimumab - Humira
- Surgical: obstruction, fistula
- Other:
- Antidiarrheal medications — loperamide, cholestyramine (chronic watery diarrhea or previous ileal resections)Ileal disease - risk of lactose intolerance
- Routine:
- Diet counseling/supplementation: Ensure adequate calcium, Vitamin D, Magnesium, Zinc, B12, iron
- Osteoporosis prevention: smoking cessation, calcium, Vit D, exercise, +/- bisphosphonate
- Immunizations UTD, yearly influenza
- Screening for colon cancer - colonoscopy q 5-10 years
- Prior to starting biologics: hepatitis serology,+/- HIV, CBC, metabolic profile with LFTS, Cr, screen for latent TB, immunizations >3 months prior to starting
- Depends on severity
Ulcerative Colitis[]
Gastroesophageal Reflux[]
- Clinical: epigastric/retrosternal burning discomfort, worse after meals (especially fatty/spicy/caffeine), worse with lying down/bending over, +/- regurge symptoms, waterbrash, dysphagia
- Extra-esophageal complications: cough, dental erosions, pulmonary fibrosis (rare), bronchitis, laryngitis, dental erosions, sinusitis
- Red flags: GI bleeding, anemia, vomiting, dysphagia, chest pain, weight loss
- Pathophysiology: lower esophageal sphincter dysfunction, delayed gastric emptying
- Complications: esophagitis, peptic stricture, Barrett's esophagus (increase risk of adenocarcinoma)
- Diagnosis: based on history and improvement with treatment. Further investigation if atypical symptoms, not relieved with medication, red flags. Consider endoscopy in patients with > 10 years of reflux.
- CBC (R/O anemia)
- GOLD STANDARD - 24 hour pH monitoring (rarely completed)
- Endoscopy (biopsy): atypical symptoms, alarm symptoms, failure to respond to treatment after 4-8 weeks of treatment, dysphagia that does not resolve within 2-4 weeks of PPI
- Treatment:
- Non-pharm: avoid spicy/citris foods, fatty foods, chocolate, caffeine, ETOH, smoking. Lose weight. Elevate head of bed. Small, frequent meals. Avoid lying down for > 2 hours post meal. Consider changing medications that affect LES tone.
- Pharm: antacids, H2 antagonists(e.g. ranitidine), PPI (e.g. pantoprazole), pro-kinetic agents (e.g.metoclopramide)
- R/A PPI in 4-8 weeks. Consider titration and then D/C at that point.
- Risk of chronic PPI use: osteoporosis, hip #, community acquired pneumonia, c.difficile, gastric acid rebound on discontinuation, iron deficiency, low magnesium, B12 deficiency
| PPI | Trade name |
|---|---|
| Omeprazole | Losec 20mg |
| Esomeprazole | Nexium 20mg |
| Rabeprazole | Pariet 20mg |
| Pantoprazole | Pantoloc/ Tecta |
| Dexlansoprazole | Dexilant |
| Lansoprazole | Prevacid 30mg |
Peptic Ulcer Disease[]
- Clinical: upper abdominal pain gnawing/burning, pain improved with meals,pain occuring 2-5 hours after a meal,nocturnal pain, nausea, bloating, early satiety
- Red flags: vomiting, UGIB, anemia, abdominal mass, unexplained weight loss, dysphagia
- Etiology: NSAIDs (often gastric), helicobacter pylori (often antral or duodenal), acid secreting tumors.
- Complications: UGIB, perforation, gastric outlet obstruction
- Investigations:
- CBC (R/O anemia) +/- FOBT
- H.Pylori: serum ELISA test (serology), Urea breath test, stool antigen test, endoscopic biopsy
- Serum ELISA testing least accurate and only useful for initial infection
- Endoscopy (>50 years old, alarm symptoms, fail treatment therapy, NSAID use)
- Acute ill CXR upright to r/o free air (perforation)
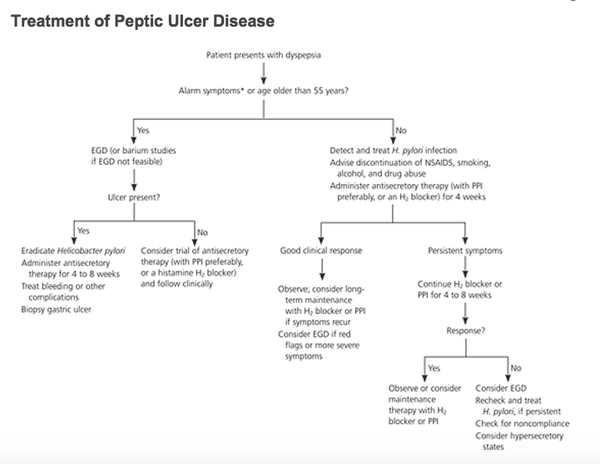
- Treatment:
- non-pharm: avoid ETOH, smoking, NSAIDs
- PPI or H2 receptor antagonist x 4 weeks then R/A
- H.Pylori treatment: combination therapy with a PPI BID (triple therapy)
- Amoxicillin 1000mg PO BID + Clarithromycin 500mg PO BID x 1 week
- Clarithromycin 500mg PO BID + Metronidazole 500mg PO BID x 1 week
- Second line: PPI BID + Metronidazole** 500mg PO BID + Amoxicillin 1000mg PO BID (note Levofloxacin 500 mg PO daily can be substituted for metronidazole in treatment refractory H. pylori)
- Quadruple therapy: PPI + bimuth + metronidazole + tetracycline x 10-14 days
- Endoscopic: bleeding sites can be ligated, clips placed, epinephrine injected
- Refractory: surgical options
- Post-treatment:
- If asymptomatic - no further investigations
- If remains symptomatic retest using urea breath test >30 days (2 weeks off PPI, 1 month of abx)
Biliary Disease[]
Risk factors[]
- F's: Fat, female, fertile, forties
Cholilithiasis (gallstones)[]
- Only 10% of people with gallstones will display symptoms
Biliary colic[]
- Clinical: RUQ pain, usually constant in nature, intense/dull discomfort, pain often associated with diaphoresis, N/V,not relieved with movement/bowel movement, often precipitated by eating a fatty meal, post-prandial pain, lasts on average 30minutes- <6 hours, afebrile, normal physical examination, normal laboratory values
- Pathophysiology: stone forced into gallbladder outlet, leading in increase in gallbladder pressure. As gallbladder relaxes, stone moves out of outlet.
- Investigations: ultrasound, (if negative and classic symptoms usually repeat U/S in 2-3 weeks). If negative could consider endoscopic ultrasound, r/o other non-biliary tree pathology
- Management: conservative management with close follow up or referral to general surgery for cholecystectomy
- Complications of cholecystectomy: bleeding, abscess formation, bile leak, biliary injury, bowel injury, chronic diarrhea
Acute Cholecystitis[]
- Clinical: biliary colic complicated by infection and inflammation of gall bladder. Assc with N/V/fever, localized peritonitis, + Murphy's sign, elevated WBC/LFTs
- Investigations: ultrasound (GB thickening, pericholecystic fluid), +/- blood cultures
- Management: admit, consult general surgery, NPO, correct electrolyte disturbances, IV fluids, analgesia, +/- Abx, NG insertion (if persistent emesis), cholecystectomy or gallbladder drainage procedures
- Selection and timing of definitive management depends on severity of symptoms, duration of symptoms, and surgical risk
- Antibiotic options:
- Ceftriaxone 1g IV q24h + Metronidazole 500mg IV/PO q8h
- Ciprofloxacin 400mg IV/500mg PO q8h + Metronidazole 500mg IV/PO q8h
Choledocholithiasis[]
- Presence of gallbladder stones in common bile duct
- Clinical: biliary type pain, elevated cholestatic liver enzymes (GGT, ALP), AST/ALT (elevated early), jaundice, courvoisier sign (palpable gallbladder often associated with malignancy)
- Uncomplicated: afebrile, N CBC
- Complicated: acute cholangitis (fever, elevated WBC), gallstone pancreatitis (elevated lipase)
- Investigations: CBC, LFTs, bilirubin, +/- blood cultures, Ultrasound (bile duct dilatation >6mm)
- Further imaging: endoscopic ultrasound, MRCP, ERCP
- Management:
- High risk: ERCP + elective cholecystectomy. Other option: cholecystectomy with intraoperative with interoperative cholangiography - followed by intraoperative or post-op ERCP
- Moderate risk: pre-op endoscopic ultrasound or MRCP
- Low risk: direct to cholecystectomy
Ascending Cholangitis[]
- Complete obstruction of infected biliary tree
- Etiology of obstruction: gallstones, strictures, malignancy, stent
- Charcot's triad: RUQ pain, fever, jaundice
- Reynold's Pentad: fever, RUQ pain, jaundice, shock, confusion
- Investigations: Elevated CBC, elevated LFTs, + blood cultures, Ultrasound (duct dilatation)
- Treatment: urgent endoscopic decompression (drainage), + broad spectrum ABx (same as cholecystitis)+ monitoring/treatment of sepsis
Pancreatitis[]
- Etiology: I GET SMASHED:' i'diopathic, gallstones, ETOH, Tumors, Scorpion bite, microbiology (mumps), Autoimmune, Surgery/Trauma (ERCP), Hypertriglyceridemia/hypercalcemia/hypotherapy, Emboli/ischemia, Drugs
- Clinical: N/V, fever, epigastric pain radiating to the back, loss of appetite, hemodynamic instability, jaundice, cullen's sign (hemorrhagic blue discolaration of umbilicus), grery turner (flank discoloration)
- Complications: ARDS, pleural effusion, pseudocyst, pancreatic abscess, pancreatic necrosis, chronic pancreatitis
Bowel Obstruction[]
Diverticulitis[]
- Imaging: CT abdo
- Management:
- Mild/moderate: fluid -->DAT, PO Abx (cipro/flagyl)
- Moderate/severe: requires imaging, consult general surgery, Abx, NPO
Appendicitis[]
- Epidemiology: M>F, highest incidence age 10-30s
- History: Periumbulical pain--> RLQ pain, fever, anorexia, N/V
- Physical: fever, RUQ tenderness
- McBurney's point (maximal tenderness 2 inches from ASIS on straight line from ASIS to umbilicus
- Rovsing's sign: pain in RLQ with palpation to LLQ
- Psoas sign (retrocecal appendix): RLQ pain with passive right hip extension
- Obturator sign (pelvic appendix): flex right hip/knee + internal rotation = RLQ pain
- Investigations/Imaging:
- Blood work: mild leukocytosis with left shift, T+S
- CT abdomen
- Ultrasound (not as specific) - could consider first line
- Management:
- Abx - cipro/flagyl or ceftriaxone/flagyl
- NPO, IVF, analgesics
- Consult general surgery for appendectomy